美國一則報導:
研究指出:壓力大會令人記憶力減退 腦部發炎
http://udn.com/news/story/5/1544652
研究發現,長期承受壓力可能造成記憶力減退,並導致腦部發炎。
科學新聞網EurekAlert!報導,美國俄亥俄州立大學研究人員在老鼠身上做實驗,利用較大的老鼠扮演入侵者,對老鼠製造壓力,研究發現,承受壓力的老鼠會記不得迷宮中的逃生出口。
研究發現,老鼠只有在一再被入侵時,才會出現失憶狀況,若只是承受1次壓力,並不會導致記憶力減退。
俄亥俄州立大學副教授高布(Jonathan Godbout)表示,「長期壓力才會導致這種狀況。承受壓力的老鼠想不起逃生出口,但沒有壓力的時候,牠們記得很清楚。」
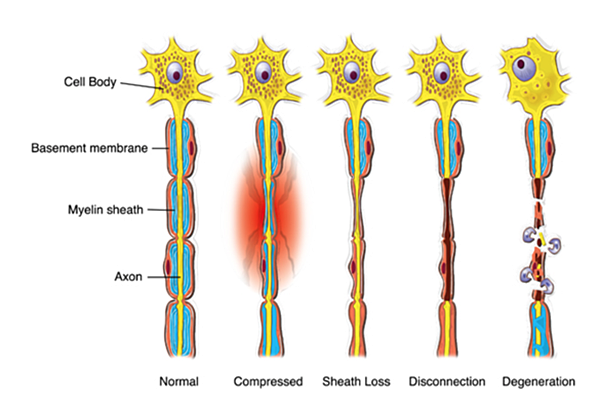
研究也發現老鼠的腦部出現變化,免疫系統在外部壓力下,導致腦部發炎。研究顯示,短期記憶障礙與腦部炎症及免疫系統有直接關聯。
研究發現,擺脫壓力後,老鼠在28天內可以恢復記憶,但有長達4星期出現迴避社交等抑鬱症狀。
高布表示,研究結果可能應用於醫治長期承受壓力的患者,例如霸凌受害者、軍人,以及被上司欺壓的員工。
研究結果刊登於「神經科學期刊」(Journal of Neuroscience)。
對照之前我在2015年的多篇文章指出
研究人員找到大腦(中樞神經系統) 和免疫系統之間的關聯性了
一個全面性的疾病:MS多發性硬化症 (歸零Reset的人生)
TED 醫學:睡眠對大腦有多重要-->靜心也是清除大腦廢物的另一種方式
都說明了 壓力和中樞神經的影響極其深遠,有時候如何釋放壓力,如何轉化壓力才是需要正視的。壓力如影隨形。
看看病友們發病的時間點,要嘛就是面臨升學考試,要不就是人生重大變故,要不就是家庭的一些事情,又或者是禍不單行,接踵而來。這些不都是因為承受著自己無法負荷的壓力而讓神經發炎的嗎?
附上原文:
http://www.eurekalert.org/pub_releases/2016-03/osu-lse022916.php
Public Release:
Long-term stress erodes memory
Study in mice places blame on immune system
Sustained stress erodes memory, and the immune system plays a key role in the cognitive impairment, according to a new study from researchers at The Ohio State University.
The work in mice could one day lead to treatment for repeated, long-term mental assault such as that sustained by bullying victims, soldiers and those who report to beastly bosses, the researchers say.
"This is chronic stress. It's not just the stress of giving a talk or meeting someone new," said lead researcher Jonathan Godbout, associate professor of neuroscience at Ohio State.
This is the first study of its kind to establish the relationship between short-term memory and prolonged stress. In the case of the mice, that meant repeat visits from a larger, nasty intruder mouse.
Mice that were repeatedly exposed to the aggressive intruder had a hard time recalling where the escape hole was in a maze they'd mastered prior to the stressful period.
"The stressed mice didn't recall it. The mice that weren't stressed, they really remembered it," Godbout said.
They also had measurable changes in their brains, including evidence of inflammation brought on by the immune system's response to the outside pressure. This was associated with the presence of immune cells, called macrophages, in the brain of the stressed mice.
The research team was able to pin the short-term memory loss on the inflammation, and on the immune system.
Their work, which appears in The Journal of Neuroscience, builds on previous research substantiating the connections between chronic stress and lasting anxiety.
The impact on memory and confirmation that the brain inflammation is caused by the immune system are important new discoveries, Godbout said.
"It's possible we could identify targets that we can treat pharmacologically or behaviorally," he said.
It could be that there are ways to interrupt the inflammation, said John Sheridan, who worked on the study and is associate director of Ohio State's Institute for Behavioral Medicine Research.
The mice used in the study are exposed to repeated social defeat - basically dominance by an alpha mouse - that aims to mimic chronic psychosocial stress experienced by humans.
Researchers at Ohio State seek to uncover the secrets behind stress and cognitive and mood problems with a long-range goal of finding ways to help those who are anxious, depressed and suffer from lasting problems, including post-traumatic stress disorder.
This new research focused on the hippocampus, a hub of memory and emotional response.
The researchers found that the stressed mice had trouble with spatial memory that resolved within 28 days. They found that the mice displayed social avoidance, which measures depressive-like behavior, that continued after four weeks of monitoring.
And they were able to measure deficits in the development of new neurons 10 days and 28 days after the prolonged stress ended.
When they gave the mice a chemical that inhibited inflammation, neither the brain-cell problem nor the depressive symptoms went away. But the memory loss and inflammatory macrophages did disappear.
And that led them to conclude that the post-stress memory trouble is directly linked to inflammation - and the immune system - rather than to other damage to the brain. That type of information can pave the way for immune-based treatments, Godbout said.
"Stress releases immune cells from the bone marrow and those cells can traffic to brain areas associated with neuronal activation in response to stress," Sheridan said. "They're being called to the brain, to the center of memory."
###
The researchers' work was supported by the National Institutes of
Health, the National Institute of Aging and the National Institute of
Dental and Craniofacial Research.Other Ohio State researchers who worked on the study were Daniel McKim, Anzela Niraula, Andrew Tarr and Eric Wohleb.
CONTACTS: Jonathan Godbout, 614-293-3456; Jonathan.Godbout@osumc.edu John Sheridan, 614-293-3571; John.Sheridan@osumc.edu
Written by: Misti Crane, 614-292-5220; Crane.11@osu.edu