大意如下:
從我開始在這個部落格寫有關CCSVI的文章已經3年了,
剛開始時,只不過是在網路上由數十位病人在網路論壇上相互辯論這一個醫療發現.
直到今天, CCSVI的議題成為由患者在社會媒介所驅動的一個現象, 已經有2萬到3萬不等的MS病人進行了這一項醫療手術. 世界各地的研究人員都正對此議題如火如荼的研究著.
而這只是揭開神秘面紗的第一步.
上星期International Society for Neurovascular Disease (ISNVD)國際神經靜脈疾病學會在佛羅里達舉行,會中長達106頁論文集中有關於CCSVI的資訊被揭露, 連結在此 (click here)
其中,是給病人最感興趣報導包含幾個CCSVI治療醫生(頁62,79,83,84,86和87的PDF可以找到)顯示出多種治療效果,包含疲勞,認知的問題,熱敏感)而且RRMS(復發緩解型)患者比PPMS或SPMS患者復原更好。
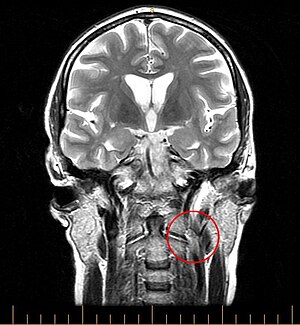
下圖右側圓圈所指為血管窄化處
原文如下:
CCSVI: Three Years On, Some Thoughts and Observations
| Image via Wikipedia |
It seems almost incredible, but it's been nearly 3 years since I wrote my first Wheelchair Kamikaze post on CCSVI (click here). At the time of that first post, CCSVI had hardly been heard of outside of some researchers in Italy and a few dozen patients debating the merits of the hypothesis on an Internet forum. Today, CCSVI has become a patient driven social media medical phenomenon. An estimated 20,000-30,000 patients have already undergone CCSVI treatment, researchers from around the world are investigating the hypothesis, and the surgical treatment of CCSVI has become a thriving industry. CCSVI has certainly come a long way, but in many ways we've only taken the first steps on what could be an epic journey.
Last week, the International Society for Neurovascular Disease (ISNVD) held its second annual scientific meeting, which lasted five full days, in Orlando, Florida. A tremendous amount of information about the nature and treatment of CCSVI was exchanged by researchers and physicians, a compendium of which can be found in a 106 page online PDF publication put out by the Society (click here).
Of most interest to patients are undoubtedly the treatment outcomes reported by several CCSVI treatment practitioners (which can be found on pages 62, 79, 83, 84, 86, and 87 of the PDF), which displayed a wide variety of treatment outcomes, but do seem to suggest several identifiable trends. It appears that quality of life issues (fatigue, cognitive issues, heat sensitivity) saw more benefit post treatment than mobility related issues, and that RRMS patients fared better than patients suffering from SPMS or PPMS. None of these studies was double blinded, all being observational and most relying on self-reported information, which can lead to inaccuracies. Still, the findings generally fall in line with some of the few double blinded studies that have been done, such as a recently completed study done in Italy (click here). CORRECTION:an anonymous reader points out that this Italian study was in fact not double blinded, and just used an independent physician to evaluate EDSS scores. Thanks for the heads up.
The meeting did bring into focus the fact that the CCSVI treatment protocol is far from standardized, with physicians varying in opinion on issues ranging from which veins to treat, whether treatment should concentrate on valves rather than the veins themselves, the use of intravascular ultrasound, and other important issues, a list of which can be found on pages 104-106 of the PDF document linked to above. There were quite a few presentations on the use of noninvasive imaging techniques (Doppler Ultrasound and MRV technology) to diagnose CCSVI, with the consensus appearing to be that neither method was especially accurate, except for extremely specialized MRV protocols that are practiced at only a few facilities. One leading CCSVI practitioner went so far as to state that he no longer requires his patients to undergo Doppler Ultrasound investigations before venoplasty, since the ultrasound results were found to be so prone to error (page 63 of the PDF).
In addition to presentations involving CCSVI treatment techniques, some important observations about the nature of the condition were also presented. The effects of reduced blood flow through the brain were discussed, as was the possible connection between bloodflow disruptions and a breakdown of the blood brain barrier, and the role of iron deposition in the MS disease process. In all, my impression (keeping in mind that I did not attend the meeting) is that the findings presented at this year's ISNVD scientific meeting were more evolutionary than revolutionary, which I suppose is something to be expected. The explosion of interest in CCSVI amongst interventional radiologists and research physicians must logically lead to attempts to fill in the many gaps of knowledge that remain in regards to CCSVI, before more dramatic leaps in understanding can be accomplished.
This eruption of interest in CCSVI within the interventional radiology community is in some ways a double-sided sword. On the plus side, it has given patients access to treatment, which in the early days was extremely hard to come by. Today, patients have their choice of treating physicians, and must do their due diligence when choosing which physician in whose hands to place themselves. As noted above, treatment techniques and philosophies vary widely from physician to physician, and patients exploring the possibility of CCSVI treatment should not be shy about asking questions in an effort to find a doctor whose treatment modality best fits their comfort level.
On the potentially negative side, CCSVI has become big business. With CCSVI treatment procedures costing about $10,000, and somewhere between 25,000-30,000 patients already treated, a little math reveals that treating CCSVI has already generated hundreds of millions of dollars in gross revenue for treating physicians. Yes, those procedures covered by medical insurance probably don't get reimbursed at the full rate charged, but this is likely made up for by patients who have undergone multiple procedures because of CCSVI's ongoing problems with restenosis. Given the fact that the number of treated patients represents only a tiny percentage of the worldwide MS population, it's easy to see that CCSVI treatment could quickly develop into a multibillion-dollar a year enterprise.
The David vs. Goliath narrative that has driven the CCSVI story thus far may soon become obsolete. To be sure, the neurology community still remains incomprehensibly steadfast in its negativity regarding CCSVI, but this is becoming counterbalanced by the enthusiasm of the interventional radiology community, and, I suspect, by the interests of the medical device manufacturers, who also stand to profit greatly should CCSVI become an accepted treatment option for MS patients. Despite the fact that very legitimate issues remain regarding the efficacy of CCSVI treatment and the lack of a consensus as to optimal interventional techniques, CCSVI treatment is being aggressively marketed by several US and international treatment facilities, which should raise some ethical questions.
Until issues with effectiveness and technique are satisfactorily answered, the CCSVI treatment procedure must be considered an experimental one, a fact that should not be lost on patients who are understandably desperate to address their illness but faced with a dizzying array of statistics, patient testimonials, and marketing efforts by for-profit ventures. In a very real way patients who choose to undergo CCSVI treatment at the current time are guinea pigs, a fact that I understood explicitly when I underwent my venoplasty back in the dark ages of CCSVI, almost two years ago. Although we've come a long way since then, in some ways the procedure remains as experimental as ever, as physicians treat a much wider array of veins much more aggressively than they did back when I underwent the procedure. Though the treatment is a minimally invasive one, it is not without risks, as is evidenced by the contingent of patients who have experienced clotting issues and vein thrombosis in the aftermath of their procedures. Indeed, one of the presentations at ISNVD highlighted a patient whose condition worsened after treatment (page 89 of the PDF), a rare occurrence to be sure, but a possibility that must factor into the decision-making process of patients considering venoplasty.
One of the most volatile controversies raging on CCSVI forums and social media sites is whether or not the condition is a cause or effect of multiple sclerosis, with those arguing for CCSVI as cause often citing the fact that the venous abnormalities being found appear to be congenital (developed in the womb) in nature. I am unsure as to the question of cause vs. effect, although I do believe that if CCSVI is a cause of MS, it is only one of many factors involved in the initiation of the disease. Even if the vascular defects being found in the veins of MS patients are congenital, this does not necessarily mean they are a cause of multiple sclerosis. There are many congenital defects that cause no adverse effect whatsoever, and I'd venture to say that many of us have some physical trait somewhere in our bodies that is outside of normal variance.
We've all heard stories of world-class athletes suddenly collapsing during or directly after extreme physical exertion. Quite often, the follow-up story is that the unfortunate athlete was a victim of a congenital heart defect, which would never have been noticed had that person not pushed his body to physical extremes. Had they not been athletes, they very well could have lived a normal life span. Likewise, a person born with congenitally abnormal ligaments in their knees might never know of their condition unless they encounter an environmental element (such as a hit to their knees) that brings their abnormality to the fore, in the form of a knee injury more severe than that which might have been suffered by a person with "normal" ligaments. Given the varied elements that have been linked to MS (infectious agents, exposure to toxins, vitamin deficiencies, genetic markers, etc.), a likely scenario is that vascular abnormalities play a part in predisposing an individual to developing MS when exposed to an unfortunate storm of other factors.
To my mind, it is becoming increasingly clear that, despite our greatest hopes, CCSVI is only a part of a much bigger and more complex MS picture. Precisely how big a part it plays is still open to question. Although CCSVI treatment does appear to benefit many patients, it has also been shown to be of little or no value to many others. CCSVI does not explain some of the factors that have previously been established about MS, such as the geographic distribution of the disease (click here), the male-female ratio that is well known to exist in MS (click here), the existence of "Multiple Sclerosis clusters" (which would seem to point to an infectious cause-click here), or the unmistakable link between MS and Epstein-Barr virus (click here). Nevertheless, CCSVI offers the promise of opening up whole new areas of research into the causes of, and treatments for, multiple sclerosis. Certainly, interested MS patients should investigate the possibility of CCSVI treatment, and make a sober assessment as to whether now is the proper time for them to jump in.
There are several ongoing research projects that should further illuminate the CCSVI picture scheduled to publish results later this year, but further robust and expeditious research is desperately needed. It is essential that we ascertain just how prevalent CCSVI is in the healthy population, gain a better understanding of the role, if any, of vascular abnormalities in the MS disease process, determine which MS patients respond best to CCSVI venoplasty, refine the techniques used to treat CCSVI, reduce the number of patients who experience restenosis, and see the development of surgical implements specifically designed to treat venous abnormalities. Neurologists need to get on board to provide interdisciplinary expertise to CCSVI studies. After all, whatever the results of the research, positive or negative, answering these questions can only be in the best interest of their patients.
CCSVI has come a long way, but there is still a long way to go. Ahankfully, the pace of CCSVI research is gaining momentum, and hopefully we will see answers to many of our questions sooner rather than later. In the meantime, my best advice is to educate yourself to the best of your ability, be your own most powerful advocate, and make treatment decisions based more on reason than emotion.






我認為這一段是比較客觀的總結:
回覆刪除在我看來,儘管我們對CCSVI抱極大的希望,但情況越來越清楚地表明,CCSVI只能說明MS這個複雜疾病的一部分。到底代表多大的一部分,目前仍然不清楚。 CCSVI治療,雖然讓許多患者受益,它也被證明對許多患者只有很少或根本沒有價值。 CCSVI無法解釋先前已建立關於MS的一些理論,比如MS疾病的地理分佈,男女比例等問題,是眾所周知存在的。在某些地區出現MS集中爆發,這似乎指向一種傳染性疾病,研究認為MS和EB病毒之間有明確無誤的聯繫。儘管如此,CCSVI對MS的成因與治療的研究開闢了一個的新領域。當然,有興趣的多發性硬化症患者應調查CCSVI治療的可能性,並作出清醒的評估,現在是否是合適的時間去做這樣的手術。
To my mind, it is becoming increasingly clear that, despite our greatest hopes, CCSVI is only a part of a much bigger and more complex MS picture. Precisely how big a part it plays is still open to question. Although CCSVI treatment does appear to benefit many patients, it has also been shown to be of little or no value to many others. CCSVI does not explain some of the factors that have previously been established about MS, such as the geographic distribution of the disease, the male-female ratio that is well known to exist in MS, the existence of "multiple sclerosis clusters" (which would seem to point to an infectious cause-, or the unmistakable link between MS and Epstein-Barr virus. Nevertheless, CCSVI offers the promise of opening up whole new areas of research into the causes of, and treatments for, multiple sclerosis. Certainly, interested MS patients should investigate the possibility of CCSVI treatment, and make a sober assessment as to whether now is the proper time for them to jump in.
相當同意,病人一定會對所有的治療方式感到希望,所以對症下藥,才是最重要的.所以CCSVI的檢驗確認是相當重要的步驟. 而血管攝影已經能夠解決這樣的問題. 剩下的就是如何做有效而且更長久的擴張了.任何一種醫療手段都需要客觀的評估,即使是藥物.
回覆刪除每種突破都是需要實驗,藥物也是.所以有很多勇者,是付出他們的勇氣決心,甚至生命,才能夠換取後人的乘涼.這是人一生當中都有可能會遇到的.運氣好的,是成熟的環境和可預期的結果.運氣不好的,是不成熟的環境和未知的未來.
所以都值得更多人繼續投入研究.
回覆刪除